Medical Assistance in Dying for Individuals with Severe Mental Illness

Sara Mohamed, MHSc, Doctor of Medicine candidate
University of British Columbia
October 09, 2023
Medical Assistance in Dying for Individuals with Severe Mental Illness
In June 2016, the Parliament of Canada passed federal legislation allowing eligible Canadian adults to request medical assistance in dying (MAiD). Since March 2021, the law no longer requires a person’s natural death to be reasonably foreseeable in order for them to access MAiD (Government of Canada, 2023). The legislation has, up to now, excluded access to MAiD for individuals suffering from mental illness. That is slated to change very soon. As of March 17, 2024, Bill C-39 states that “persons suffering solely from a mental illness will be eligible for MAID” (Department of Justice Canada, 2023).
MAiD has been and continues to be a controversial topic in Canada, as compared to countries such as Switzerland, Netherlands, and Belgium that have allowed assisted dying since the early 2000s, or mid-1900s in the case of Switzerland (Dying with Dignity, 2021). These regions also already allow MAiD requested by persons with mental illness, on the basis of suffering from that condition (Doelle, 2022).
In Canada, concerns remain with respect to the planned extension of MAiD to people requesting this service on the basis of their suffering related to mental illness. Certainly, the nature and course of mental illness can add a layer of complexity to fears or arguments against MAiD usage more generally. Some of the arguments that exist in favor of and against MAiD that are not specific to people suffering from mental illness include:
|
Arguments in favor of MAiD |
Arguments opposing MAiD |
|
It allows a person to practice their right to autonomy; a person has a right to have the power to make their own choices and thus should be able to die and have the means to do so |
The power imbalance between healthcare providers and patients -providers may exert influence on patients that can make patients feel as if they don’t have any other therapeutic options left |
|
Dignity and control – it gives a person a choice on how to die |
Religious and cultural concerns |
|
It will prevent suffering, which can be viewed as part of the physician’s Hippocratic oath to “Do no harm” |
Ending someone’s life could be considered acting against the Hippocratic oath to “Do no harm” |
|
Regulation- it can prevent additional danger created by illegal markets and provide a safe means for an individual to die |
Performing MAiD can have a negative emotional toll on healthcare providers |
|
Can reduce healthcare costs |
|
Table 1: Arguments in favor and opposing MAiD
The arguments above can apply to MAiD for those suffering from mental illness, but there are also some more specific considerations to be made when considering this population. A primary argument in favor of extending the service to individuals who are suffering from mental illness is that we avoid excluding a population from accessing a form of health care (Dembo, 2021). From this point of view, competent individuals with mental disorders should be able to participate in making healthcare decisions, including those that can result in death (Dembo, 2021). Concerns specific to MAiD for people who suffer from mental illness include the possibility that the request can stem from symptoms of the mental illness (Appelbaum, 2018). Assessing the capacity of the patient can be difficult, as symptoms of the mental illness can interfere with the ability to understand or appreciate the nature or consequences of treatment decisions (Government of Canada, 2021). Further, the trajectory of mental illness is harder to predict than those of physical disease (Government of Canada, 2021), as mental health fluctuates with highs and lows. With this in mind, there will always be a degree of uncertainty with MAiD for those suffering from mental illness, which can be frightening as the choice is life or death (van Veen et al., 2022).
Other concerns regarding extending eligibility of MAiD for those suffering from mental illness involve stigma and structural vulnerability. Some have proposed extending MAiD to this population could send a message that individuals with mental illness have lives that are more expendable than individuals not grasping with mental illness. Healthcare providers may perceive MAiD for those with mental illness as offering “permission” to give up the provision of care for patients with difficult cases of mental illness and use MAiD as their only option (Appelbaum, 2018). This frame of thought can also be present among those seeking the service as MAiD may become a consideration when they cannot get the mental health care they need, which is a valid concern with the inequities that exist across Canada in accessing evidence-informed mental health care and treatment (CAMH, 2023). This concern is exacerbated since people with mental illness are overrepresented among those who live in poverty or experience homelessness and are disadvantaged when it comes to mental health care access. This brings up the thought of whether the extension of MAiD to those who suffer from mental illness is premature (Mahendiran, 2021) if mental health care in Canada still needs dramatic improvements.
Palliative psychiatry
Palliative care aims to optimize quality of life and reduce suffering among individuals with serious, complex, and often terminal illnesses. This contrasts with MAiD through the method by which suffering is reduced, as MAiD aims to reduce suffering by helping an eligible individual end their life when they request it. It is argued that access to palliative care to alleviate a person’s suffering is a necessity for a request for physician-assisted death to truly be voluntary (Garneau & Martin, 2023). Preliminary evidence also suggests that improved palliative care strategies and services for individuals with severe and persistent mental illness may lead to fewer requests for assisted dying (Trachsel et al., 2016). An important aspect of palliative psychiatry is the acceptance that the approach is not curative, but rather used to help stabilize or improve quality of life without necessarily having an impact on the disease progression in the long term (Trachsel et al., 2016). Features of palliative psychiatry are provided in Figure 1.
Significant debate exists around whether MAiD should be considered part of palliative care. Those against this highlight the important difference that palliative care allows healthcare providers to focus on providing high-quality care and relief of suffering as death takes its natural course, which may be relevant for the sake of the conscience and integrity of palliative care providers (Association for Reformed Political Action, n.d.) In contrast, MAiD assessors and providers believe that both services aim to relieve suffering and focus on patient-centered care, and thus should be integrated with palliative care (Association for Reformed Political Action, n.d.)
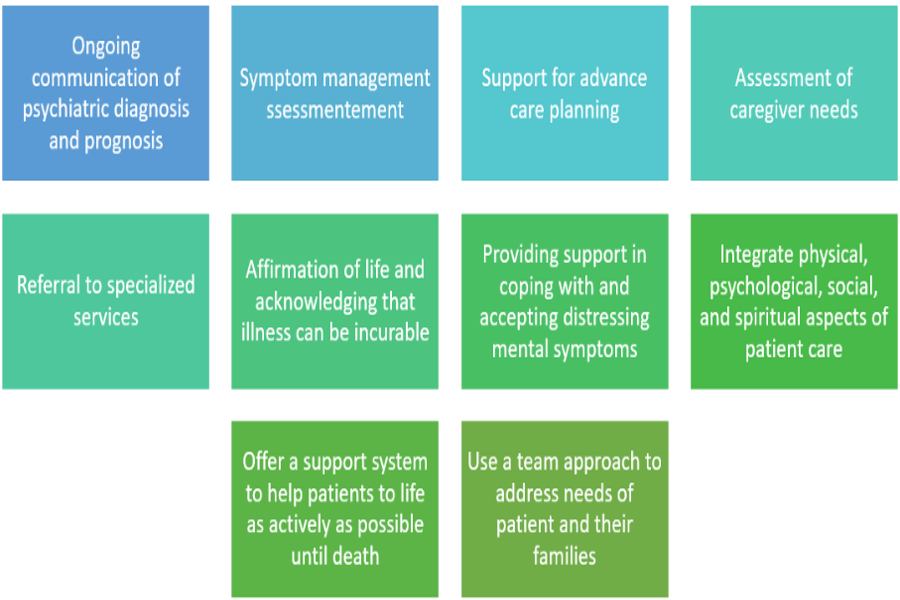
Figure 1: Features of palliative psychiatry (Trachsel et al., 2016)
Final note
Medical assistance in dying is a complex issue in and of itself. However, many of the concerns or negative outcomes related to legalizing MAiD for individuals suffering solely from mental illness can be avoided with the development of appropriate and comprehensive standards of practice for each step in the MAiD process and beyond. With appropriate standards of care, eligibility requirements, and methods of assessment in place, can MAiD simply be considered an effort to promote patient-centered care?
To learn more …
About the process of MAiD: https://www.canada.ca/en/health-canada/services/medical-assistance-dying.html
About eligibility criteria: https://www.justice.gc.ca/eng/csj-sjc/pl/ad-am/c7/p3.html
References
Appelbaum, P. S. (2018). Physician‐assisted death in psychiatry. World Psychiatry, 17(2), 145. https://doi.org/10.1002/wps.20548
Association for Reformed Political Action. (n.d.). Merging palliative care and MAID. ARPA Canada Merging palliative care and MAiD Comments. Retrieved April 27, 2023, from https://arpacanada.ca/articles/merging-palliative-care-and-maid/
CAMH. (2023, February). Medical assistance in dying (maid) and mental illness – FAQs. CAMH. Retrieved April 22, 2023, from https://www.camh.ca/en/camh-news-and-stories/maid-and-mental-illness-faqs
Dembo, J. (2021, February 2). Brief Submitted to Standing Committee on Legal and Constitutional Affairs Re: Bill C-7, Criminal Code Amendments (medical assistance in dying). https://sencanada.ca/. https://sencanada.ca/content/sen/committee/432/LCJC/Briefs/Brief_JustineDembo_e.pdf
Department of Justice Canada. (2023, March 9). Eligibility for medical assistance in dying for persons suffering solely from mental illness extended to March 17, 2024. Canada.ca. https://www.canada.ca/en/department-justice/news/2023/03/eligibility-for-medical-assistance-in-dying-for-persons-suffering-solely-from-mental-illness-extended-to-march-17-2024.html
Doelle, A. (2022, October 28). Medical assistance in dying around the world. Dying With Dignity Canada. Retrieved April 24, 2023, from https://www.dyingwithdignity.ca/blog/medical-assistance-in-dying-around-the-world/#:~:text=Many%20countries%2C%20including%20the%20Netherlands,of%20MAID%20around%20the%20world
Dying with Dignity. (2021, September 11). Assisted dying around the world. Dying With Dignity Canada. Retrieved April 26, 2023, from https://www.dyingwithdignity.ca/education- resources/assisted_dying_around_the_world_recording_september2021/#_ftn6
Garneau, M., & Martin, Y. (2023, February). Medical assistance in dying in Canada: Choice for Canadians. Parliament of Canada. https://www.parl.ca/Content/Committee/441/AMAD/Reports/RP12234766/amadrp02/amadrp02-e.pdf
Government of Canada. (2021, September 1). Part II – Eligibility Criteria for MAID. Department of Justice. Retrieved April 26, 2023, from https://www.justice.gc.ca/eng/csj-sjc/pl/ad-am/c7/p3.html.
Government of Canada. (2023, March 27). Medical assistance in dying. Canada.ca. Retrieved April 26, 2023, from https://www.canada.ca/en/health-canada/services/medical- assistance-dying.html
Mahendiran, M. (2021, September 7). Mental health and MAID: An ongoing challenge. Healthy Debate. Retrieved April 26, 2023, from https://healthydebate.ca/2021/09/topic/mental- health-and-maid/
Ontario Palliative Care Network. (n.d.). Palliative Care Concepts and terms. Palliative Care Concepts and Terms | Ontario Palliative Care Network. Retrieved April 23, 2023, from https://www.ontariopalliativecarenetwork.ca/about-palliative-care/concepts-terms#:~:text=Palliative%20care%20focuses%20on%20improving,request%20it%2C%20by%20administering%20medications.
Trachsel, M., Irwin, S.A., Biller-Andorno, N. et al. Palliative psychiatry for severe persistent mental illness as a new approach to psychiatry? Definition, scope, benefits, and risks. BMC Psychiatry 16, 260 (2016). https://doi.org/10.1186/s12888-016-0970-y
van Veen, S. M., Ruissen, A. M., Beekman, A. T., Evans, N., & Widdershoven, G. A. (2022). Establishing irremediable psychiatric suffering in the context of medical assistance in dying in the Netherlands: a qualitative study. CMAJ, 194(13), E485-E491. doi: 10.1503/cmaj.210929
Photo by National Cancer Institute on Unsplash
