Lessons from the COVID-19 Pandemic: Technology in Public Health Surveillance
Mahabbah Mirza
Master of Health Sciences in Global Health Systems
March 18, 2024
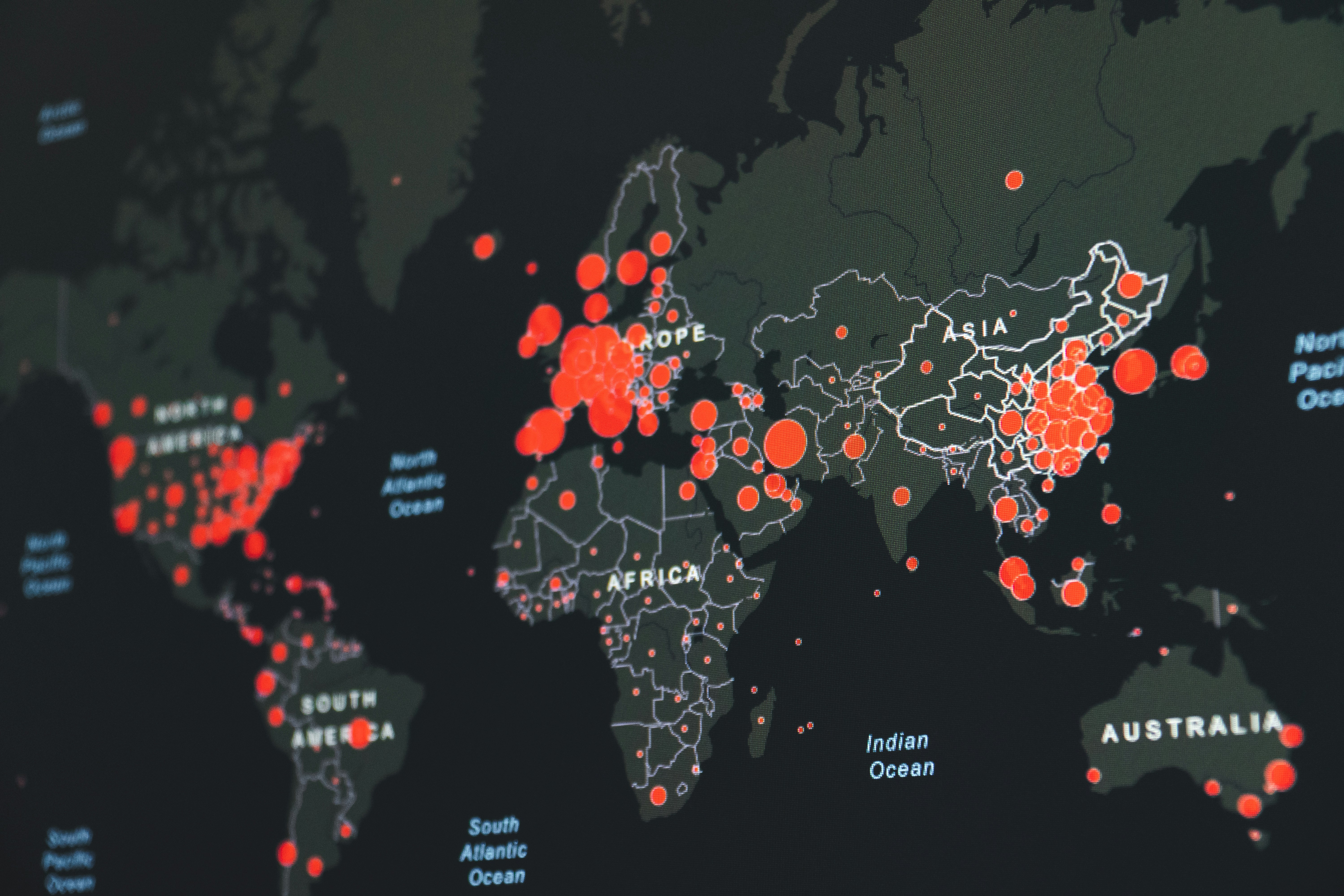
During the COVID-19 pandemic, I recall the strain on our Canadian public healthcare system and its greatest ally: Technology. The COVID-19 Alert App was one of the many technological advances that played a pivotal role in curbing cases and reshaping our surveillance methods. Through rapid notifications of potential exposures, we had faster and wider contact tracing than traditional surveillance methods. Given the 6.9 million downloads and 57,000 users actively tracing contacts (Government of Canada, 2022), technology had an evident impact - it was not just changing public health surveillance but was the game changer itself.
Public health surveillance is a routine process of gathering, analyzing, and interpreting data on diseases and health interventions to inform public health responses (National Collaborating Centre for Methods and Tool, 2023). In the last two decades, it has evolved through the emergence of new diseases and the introduction of new technologies (Public Health Agency of Canada, 2023). The capabilities of surveillance in any system depend on many factors, including the quality of its tools. The rise of digital technology is revolutionizing what is possible for public health: accelerating the development of epidemiology and transforming how we monitor and respond to health challenges (Kostkova et al., 2021). This transformation can be seen in the evolution of smartphones from mere communication devices into revolutionary tools that can detect, monitor, and respond to infectious diseases with greater efficiency and accuracy, both locally and globally. For example, a smartphone-controlled biosensor in India was developed to diagnose COVID-19 using a paper strip and a CRISPR-based technique. The smartphone app can capture the image of the strip, quantify the signal using machine learning, and upload the results to a cloud. This device is portable, affordable, fast, and can be used in resource-limited settings or at home (Ma et al., 2023).
In efforts to combat outbreaks, slow reporting methods, such as manual data collection, are inefficient and delay the identification of viral spreads. In the case of COVID-19, the virus had already spread within communities by the time the data reached public health authorities (Kostkova et al., 2021). Even in China, COVID-19 outbreaks were initially tracked based on confirmed cases from doctors, not including rapid-at-home test results. Typically, doctors detect disease outbreaks by observing unusual symptom patterns in patients. However, these patterns can vary, requiring repeated observation and testing (Dai & Wang, 2020). The delay in recognizing the widespread transmission of COVID-19 and new cases reiterates the limitations of relying solely on current symptom monitoring and confirmed case-reporting methods to timely signal an epidemic.
Integrating technology into health surveillance systems is a promising solution for detecting health threats at early stages. Mobile health applications (mHealth apps) have emerged as powerful tools for improving population health literacy. Through mobile devices, mHealth apps offer preventive healthcare education, disease surveillance, treatment support, outbreak tracking, and chronic disease management (Holman, 2018). Furthermore, apps equipped with Bluetooth technology, like the COVID-19 Alert App, facilitate contact tracing efforts by health authorities. As data becomes more widely available, healthcare professionals can easily reach patients and create a network to control epidemics.
However, technology implementation for public health surveillance faces various limitations. One such limitation is the lack of standardized methods for collecting and sharing data (Public Health Agency of Canada, 2023). Worldwide, apps with Bluetooth technology have been met with distrust and resistance, based on the belief that data will be sold to private companies or will be monitored beyond the app’s stated timeframe (Kostkova et al., 2021). I remember the skepticism surrounding the COVID-19 Alert App here in Canada, mainly due to concerns about the government misusing the data collected. Despite being assured that the app was temporarily monitoring data, many were still deterred from using it (Oyibo & Morita, 2021). In addition to privacy concerns, there are global disparities in funding allocation for technology. High-income countries (HICs) dominate global health research funding and primarily allocate resources to institutions within their own borders (Charani et al., 2023). This results in a divide where HICs can develop technology tailored to their specific cultures and healthcare systems, while low-income countries (LICs) receive minimal research and attention. The need for context-specific contact tracing is particularly difficult in LICs due to limited access to formal healthcare systems and diagnostic facilities, posing challenges in implementing technology-driven public health surveillance.
Despite challenges, public health surveillance methods continually adapt to serve the population. Integrating technology signifies a change in our approaches to disease preparedness and response. Addressing privacy and equity concerns in technology research is vital for promoting a globally inclusive approach to public health. By overcoming these barriers, we can fully leverage surveillance technology to detect, monitor, and respond to health challenges effectively locally and globally.
References
Charani, E., Abimbola, S., Pai, M., Adeyi, O., Mendelson, M., Laxminarayan, R., & Rasheed, M. (2023). Funders: The missing link in equitable global health research? The Global Health Network Conference Proceedings 2022. https://doi.org/10.21428/3d48c34a.a089d34e
Dai, Y., Wang, J. (2020). Identifying the outbreak signal of covid-19 before the response of the traditional disease monitoring system. PLOS Neglected Tropical Diseases, 14(10). https://doi.org/10.1371/journal.pntd.0008758
Government of Canada. (2022, July 14). Statement from Health Canada on decommissioning covid alert. Government of Canada. https://www.canada.ca/en/health-canada/news/2022/06/statement-from-health-canada-on-decommissioning -covid-alert.html
Holman, T. (2018, November 29). mHealth (mobile health). Health IT. https://www.techtarget.com/searchhealthit/definition/mHealth
Kostkova, P., Saigí-Rubió, F., Eguia, H., Borbolla, D., Verschuuren, M., Hamilton, C., Azzopardi-Muscat, N., & Novillo-Ortiz, D. (2021). Data and digital solutions to support surveillance strategies in the context of the COVID-19 pandemic. Frontiers in Digital Health, 3. https://doi.org/10.3389/fdgth.2021.707902
Ma, Y., Luo, Y., Feng, X., Huang, C., & Shen, X. (2023). Smartphone-controlled biosensor for viral respiratory infectious diseases: Screening and response. Talanta, 254, 124167. https://doi.org/10.1016/j.talanta.2022.124167
National Collaborating Centre for Methods and Tools. (2023, September 15). What are the latest innovations in public health surveillance? https://nccmt.ca/pdfs/res/surveillance-innovations.
Oyibo, K., & Morita, P. P. (2021). Designing better exposure notification apps: The role of persuasive design. JMIR Public Health and Surveillance, 7(11). https://doi.org/10.2196/28956
Public Health Agency of Canada. (2023, November 20). A vision for public health surveillance in Canada by 2030: Technical discussion guide. Government of Canada. https://www.canada.ca/en/public-health/programs/consultation-vision-public-health-assessment-canada-future/document-technical.html
Photo by Martin Sanchez on Unsplash
